Mri Scanner Is Controlled by Computer Hardware
| Magnetic resonance imaging | |
|---|---|
| Para-sagittal MRI of the caput, with aliasing artifacts (nose and forehead appear at the back of the caput) | |
| Synonyms | Nuclear magnetic resonance imaging (NMRI), magnetic resonance tomography (MRT) |
| ICD-9-CM | 88.91 |
| MeSH | D008279 |
| MedlinePlus | 003335 |
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from CT and PET scans. MRI is a medical application of nuclear magnetic resonance (NMR) which tin can also be used for imaging in other NMR applications, such as NMR spectroscopy.
MRI is widely used in hospitals and clinics for medical diagnosis, staging and follow-up of illness. Compared to CT, MRI provides better dissimilarity in images of soft-tissues, e.g. in the brain or belly. However, it may exist perceived as less comfortable past patients, due to the usually longer and louder measurements with the discipline in a long, circumscribed tube. Additionally, implants and other non-removable metallic in the trunk can pose a risk and may exclude some patients from undergoing an MRI exam safely.
MRI was originally chosen NMRI (nuclear magnetic resonance imaging), simply "nuclear" was dropped to avert negative associations.[i] Certain atomic nuclei are able to absorb radio frequency energy when placed in an external magnetic field; the resultant evolving spin polarization can induce a RF bespeak in a radio frequency coil and thereby be detected.[2] In clinical and research MRI, hydrogen atoms are most often used to generate a macroscopic polarization that is detected by antennae close to the subject being examined.[2] Hydrogen atoms are naturally arable in humans and other biological organisms, peculiarly in water and fat. For this reason, most MRI scans substantially map the location of h2o and fatty in the body. Pulses of radio waves excite the nuclear spin energy transition, and magnetic field gradients localize the polarization in space. By varying the parameters of the pulse sequence, different contrasts may exist generated between tissues based on the relaxation properties of the hydrogen atoms therein.
Since its development in the 1970s and 1980s, MRI has proven to exist a versatile imaging technique. While MRI is nigh prominently used in diagnostic medicine and biomedical enquiry, it besides may be used to class images of non-living objects, such as mummies. Diffusion MRI and Functional MRI extends the utility of MRI to capture neuronal tracts and blood period respectively in the nervous system, in addition to detailed spatial images. The sustained increment in demand for MRI within health systems has led to concerns about cost effectiveness and overdiagnosis.[3] [4] [ dubious ]
Mechanism [edit]
Construction and physics [edit]

Schematic of construction of a cylindrical superconducting MR scanner
In most medical applications, hydrogen nuclei, which consist solely of a proton, that are in tissues create a point that is processed to form an prototype of the body in terms of the density of those nuclei in a specific region. Given that the protons are affected by fields from other atoms to which they are bonded, it is possible to separate responses from hydrogen in specific compounds. To perform a study, the person is positioned within an MRI scanner that forms a strong magnetic field around the area to be imaged. Showtime, energy from an oscillating magnetic field is temporarily applied to the patient at the advisable resonance frequency. Scanning with X and Y gradient coils causes a selected region of the patient to experience the verbal magnetic field required for the energy to be absorbed. The atoms are excited by a radio frequency (RF) pulse and the resultant signal is measured by a receiving coil. The RF indicate may be processed to deduce position information by looking at the changes in RF level and phase caused past varying the local magnetic field using gradient coils. As these coils are apace switched during the excitation and response to perform a moving line scan, they create the characteristic repetitive racket of an MRI scan as the windings move slightly due to magnetostriction. The contrast betwixt unlike tissues is determined past the rate at which excited atoms return to the equilibrium state. Exogenous contrast agents may exist given to the person to brand the image clearer.[5]
The major components of an MRI scanner are the main magnet, which polarizes the sample, the shim coils for correcting shifts in the homogeneity of the principal magnetic field, the slope system which is used to localize the region to be scanned and the RF arrangement, which excites the sample and detects the resulting NMR indicate. The whole system is controlled by i or more than computers.

A mobile MRI unit visiting Glebefields Health Eye, Tipton, England
MRI requires a magnetic field that is both strong and uniform to a few parts per million across the scan book. The field force of the magnet is measured in teslas – and while the majority of systems operate at 1.v T, commercial systems are bachelor between 0.2 and 7 T. Most clinical magnets are superconducting magnets, which require liquid helium to go on them very cold. Lower field strengths can be achieved with permanent magnets, which are often used in "open" MRI scanners for claustrophobic patients.[half-dozen] Lower field strengths are also used in a portable MRI scanner approved by the FDA in 2020.[vii] Recently, MRI has been demonstrated also at ultra-low fields, i.east., in the microtesla-to-millitesla range, where sufficient signal quality is fabricated possible by prepolarization (on the order of 10–100 mT) and by measuring the Larmor precession fields at about 100 microtesla with highly sensitive superconducting breakthrough interference devices (SQUIDs).[viii] [9] [x]
T1 and T2 [edit]
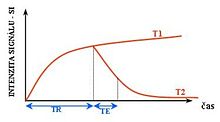
Furnishings of TR and TE on MR signal

Examples of T1-weighted, T2-weighted and PD-weighted MRI scans
Each tissue returns to its equilibrium state later excitation past the contained relaxation processes of T1 (spin-lattice; that is, magnetization in the same management as the static magnetic field) and T2 (spin-spin; transverse to the static magnetic field). To create a T1-weighted paradigm, magnetization is immune to recover before measuring the MR signal by changing the repetition time (TR). This epitome weighting is useful for assessing the cerebral cortex, identifying fatty tissue, characterizing focal liver lesions, and in full general, obtaining morphological information, as well as for post-contrast imaging. To create a T2-weighted image, magnetization is allowed to decay before measuring the MR indicate by changing the echo time (TE). This image weighting is useful for detecting edema and inflammation, revealing white thing lesions, and assessing zonal anatomy in the prostate and uterus.
The standard display of MRI images is to represent fluid characteristics in black and white images, where different tissues turn out equally follows:
| Signal | T1-weighted | T2-weighted |
|---|---|---|
| High |
|
|
| Inter- mediate | Grayness matter darker than white affair[13] | White matter darker than grey affair[13] |
| Low |
|
|
Diagnostics [edit]
Usage by organ or system [edit]

Patient being positioned for MR study of the head and abdomen
MRI has a wide range of applications in medical diagnosis and more than 25,000 scanners are estimated to be in use worldwide.[fourteen] MRI affects diagnosis and handling in many specialties although the result on improved health outcomes is disputed in sure cases.[fifteen] [16]
MRI is the investigation of choice in the preoperative staging of rectal and prostate cancer and has a function in the diagnosis, staging, and follow-upward of other tumors,[17] equally well equally for determining areas of tissue for sampling in biobanking.[18] [xix]
Neuroimaging [edit]

MRI is the investigative tool of option for neurological cancers over CT, equally information technology offers better visualization of the posterior cranial fossa, containing the brainstem and the cerebellum. The dissimilarity provided between gray and white thing makes MRI the best pick for many weather condition of the central nervous system, including demyelinating diseases, dementia, cerebrovascular disease, infectious diseases, Alzheimer'south illness and epilepsy.[20] [21] [22] Since many images are taken milliseconds apart, it shows how the encephalon responds to different stimuli, enabling researchers to written report both the functional and structural brain abnormalities in psychological disorders.[23] MRI too is used in guided stereotactic surgery and radiosurgery for treatment of intracranial tumors, arteriovenous malformations, and other surgically treatable conditions using a device known equally the N-localizer.[24] [25] [26] New Artificial intelligence in healthcare tools have demonstrated higher image quality and morphometric analysis in neuroimaging with the application of a denoising organisation.[27]
Cardiovascular [edit]

MR angiogram in congenital centre disease
Cardiac MRI is complementary to other imaging techniques, such as echocardiography, cardiac CT, and nuclear medicine. It can exist used to assess the structure and the role of the heart.[28] Its applications include cess of myocardial ischemia and viability, cardiomyopathies, myocarditis, iron overload, vascular diseases, and congenital heart affliction.[29]
Musculoskeletal [edit]
Applications in the musculoskeletal organisation include spinal imaging, assessment of joint disease, and soft tissue tumors.[30] Also, MRI techniques tin be used for diagnostic imaging of systemic muscle diseases including genetic musculus diseases.[31] [32]
Swallowing motility of throat and oesophagus tin cause movement artifact over the imaged spine. Therefore, a saturation pulse[ clarification needed ] applied over this region the throat and oesophagus tin help to avoid this antiquity. Motility antiquity arising due to pumping of the center can be reduced by timing the MRI pulse according to middle cycles. [33] Blood vessels flow artifacts can be reduced by applying saturation pulses above and below the region of interest.[34]
Liver and gastrointestinal [edit]
Hepatobiliary MR is used to notice and characterize lesions of the liver, pancreas, and bile ducts. Focal or diffuse disorders of the liver may be evaluated using diffusion-weighted, opposed-phase imaging and dynamic contrast enhancement sequences. Extracellular dissimilarity agents are used widely in liver MRI, and newer hepatobiliary dissimilarity agents also provide the opportunity to perform functional biliary imaging. Anatomical imaging of the bile ducts is achieved past using a heavily T2-weighted sequence in magnetic resonance cholangiopancreatography (MRCP). Functional imaging of the pancreas is performed following administration of secretin. MR enterography provides non-invasive assessment of inflammatory bowel disease and minor bowel tumors. MR-colonography may play a role in the detection of large polyps in patients at increased risk of colorectal cancer.[35] [36] [37] [38]
Angiography [edit]
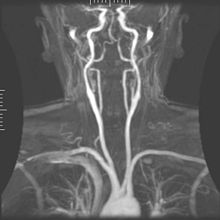
Magnetic resonance angiography
Magnetic resonance angiography (MRA) generates pictures of the arteries to evaluate them for stenosis (aberrant narrowing) or aneurysms (vessel wall dilatations, at risk of rupture). MRA is ofttimes used to evaluate the arteries of the neck and encephalon, the thoracic and abdominal aorta, the renal arteries, and the legs (called a "run-off"). A variety of techniques can be used to generate the pictures, such as assistants of a paramagnetic contrast agent (gadolinium) or using a technique known as "flow-related enhancement" (e.g., 2d and 3D fourth dimension-of-flight sequences), where near of the signal on an image is due to blood that recently moved into that plane (run into besides Flash MRI).[39]
Techniques involving phase aggregating (known equally phase contrast angiography) tin also exist used to generate flow velocity maps easily and accurately. Magnetic resonance venography (MRV) is a like procedure that is used to image veins. In this method, the tissue is now excited inferiorly, while the signal is gathered in the plane immediately superior to the excitation plane—thus imaging the venous blood that recently moved from the excited aeroplane.[forty]
Contrast agents [edit]
MRI for imaging anatomical structures or claret flow practice not require contrast agents since the varying properties of the tissues or blood provide natural contrasts. Nonetheless, for more specific types of imaging, exogenous contrast agents may exist given intravenously, orally, or intra-articularly.[5] The nearly commonly used intravenous contrast agents are based on chelates of gadolinium.[41] In general, these agents have proved safer than the iodinated dissimilarity agents used in X-ray radiography or CT. Anaphylactoid reactions are rare, occurring in approx. 0.03–0.1%.[42] Of particular involvement is the lower incidence of nephrotoxicity, compared with iodinated agents, when given at usual doses—this has made contrast-enhanced MRI scanning an pick for patients with renal harm, who would otherwise not be able to undergo contrast-enhanced CT.[43]
Gadolinium-based contrast reagents are typically octadentate complexes of gadolinium(3). The complex is very stable (log K > 20) so that that, in use, the concentration of the united nations-complexed Gdiii+ ions should exist below the toxicity limit. The ninth place in the metal ion's coordination sphere is occupied by a water molecule which exchanges rapidly with water molecules in the reagent molecule's firsthand surroundings, affecting the magnetic resonance relaxation time.[44] For details run across MRI contrast agent.
In Dec 2017, the Food and Drug Assistants (FDA) in the United states appear in a drug prophylactic advice that new warnings were to exist included on all gadolinium-based dissimilarity agents (GBCAs). The FDA also chosen for increased patient didactics and requiring gadolinium contrast vendors to deport boosted animal and clinical studies to appraise the rubber of these agents.[45] Although gadolinium agents have proved useful for patients with kidney impairment, in patients with severe kidney failure requiring dialysis there is a risk of a rare but serious affliction, nephrogenic systemic fibrosis, which may be linked to the use of certain gadolinium-containing agents. The virtually often linked is gadodiamide, but other agents accept been linked too.[46] Although a causal link has non been definitively established, current guidelines in the United States are that dialysis patients should but receive gadolinium agents where essential and that dialysis should exist performed as soon equally possible after the scan to remove the agent from the torso promptly.[47] [48]
In Europe, where more gadolinium-containing agents are bachelor, a classification of agents co-ordinate to potential risks has been released.[49] [50] In 2008, a new contrast agent named gadoxetate, brand name Eovist (U.s.a.) or Primovist (Eu), was canonical for diagnostic use: This has the theoretical do good of a dual excretion path.[51]
Sequences [edit]
An MRI sequence is a item setting of radiofrequency pulses and gradients, resulting in a detail image advent.[52] The T1 and T2 weighting tin can too be described as MRI sequences.
Overview table
This table does not include uncommon and experimental sequences.
| Group | Sequence | Abbr. | Physics | Main clinical distinctions | Example |
|---|---|---|---|---|---|
| Spin echo | T1 weighted | T1 | Measuring spin–lattice relaxation by using a brusk repetition time (TR) and echo time (TE). |
Standard foundation and comparing for other sequences |  |
| T2 weighted | T2 | Measuring spin–spin relaxation past using long TR and TE times |
Standard foundation and comparison for other sequences |  | |
| Proton density weighted | PD | Long TR (to reduce T1) and curt TE (to minimize T2).[56] | Articulation disease and injury.[57]
|  | |
| Gradient echo (GRE) | Steady-state gratuitous precession | SSFP | Maintenance of a steady, rest transverse magnetisation over successive cycles.[59] | Creation of cardiac MRI videos (pictured).[59] |  |
| Effective T2 or "T2-star" | T2* | Spoiled gradient recalled echo (GRE) with a long echo time and pocket-sized flip angle[60] | Low point from hemosiderin deposits (pictured) and hemorrhages.[lx] |  | |
| Susceptibility-weighted | SWI | Spoiled gradient recalled echo (GRE), fully flow compensated, long echo time, combines phase image with magnitude epitome[61] | Detecting small amounts of hemorrhage (diffuse axonal injury pictured) or calcium.[61] |  | |
| Inversion recovery | Short tau inversion recovery | STIR | Fat suppression past setting an inversion time where the signal of fat is zero.[62] | High signal in edema, such as in more than astringent stress fracture.[63] Shin splints pictured: |  |
| Fluid-adulterate inversion recovery | FLAIR | Fluid suppression past setting an inversion time that nulls fluids | High signal in lacunar infarction, multiple sclerosis (MS) plaques, subarachnoid bleeding and meningitis (pictured).[64] |  | |
| Double inversion recovery | DIR | Simultaneous suppression of cerebrospinal fluid and white thing past 2 inversion times.[65] | High signal of multiple sclerosis plaques (pictured).[65] |  | |
| Diffusion weighted (DWI) | Conventional | DWI | Measure of Brownian motion of water molecules.[66] | High signal within minutes of cognitive infarction (pictured).[67] |  |
| Apparent diffusion coefficient | ADC | Reduced T2 weighting by taking multiple conventional DWI images with different DWI weighting, and the change corresponds to diffusion.[68] | Low betoken minutes later cognitive infarction (pictured).[69] |  | |
| Diffusion tensor | DTI | Mainly tractography (pictured) by an overall greater Brownian motion of water molecules in the directions of nerve fibers.[70] |
|  | |
| Perfusion weighted (PWI) | Dynamic susceptibility contrast | DSC | Measures changes over fourth dimension in susceptibility-induced signal loss due to gadolinium contrast injection.[72] |
|  |
| Arterial spin labelling | ASL | Magnetic labeling of arterial claret below the imaging slab, which subsequently enters the region of interest.[74] Information technology does not need gadolinium contrast.[75] | |||
| Dynamic contrast enhanced | DCE | Measures changes over time in the shortening of the spin–lattice relaxation (T1) induced past a gadolinium dissimilarity bolus.[76] | Faster Gd contrast uptake along with other features is suggestive of malignancy (pictured).[77] |  | |
| Functional MRI (fMRI) | Blood-oxygen-level dependent imaging | BOLD | Changes in oxygen saturation-dependent magnetism of hemoglobin reflects tissue activity.[78] | Localizing brain activity from performing an assigned job (due east.yard. talking, moving fingers) earlier surgery, also used in inquiry of cognition.[79] |  |
| Magnetic resonance angiography (MRA) and venography | Time-of-flight | TOF | Blood entering the imaged area is not nevertheless magnetically saturated, giving it a much higher betoken when using short repeat time and flow bounty. | Detection of aneurysm, stenosis, or dissection[lxxx] |  |
| Phase-dissimilarity magnetic resonance imaging | PC-MRA | Ii gradients with equal magnitude, but opposite management, are used to encode a phase shift, which is proportional to the velocity of spins.[81] | Detection of aneurysm, stenosis, or dissection (pictured).[80] |  (VIPR) |
Other specialized configurations [edit]
Magnetic resonance spectroscopy [edit]
Magnetic resonance spectroscopy (MRS) is used to measure the levels of unlike metabolites in body tissues, which can be achieved through a variety of single voxel or imaging-based techniques.[82] The MR indicate produces a spectrum of resonances that corresponds to dissimilar molecular arrangements of the isotope being "excited". This signature is used to diagnose certain metabolic disorders, peculiarly those affecting the encephalon,[83] and to provide information on tumor metabolism.[84]
Magnetic resonance spectroscopic imaging (MRSI) combines both spectroscopic and imaging methods to produce spatially localized spectra from within the sample or patient. The spatial resolution is much lower (express past the available SNR), merely the spectra in each voxel contains information about many metabolites. Because the available signal is used to encode spatial and spectral data, MRSI requires high SNR achievable only at higher field strengths (3 T and above).[85] The loftier procurement and maintenance costs of MRI with extremely high field strengths[86] inhibit their popularity. However, contempo compressed sensing-based software algorithms (e.g., SAMV[87]) have been proposed to accomplish super-resolution without requiring such high field strengths.
Real-time MRI [edit]
Real-time MRI of a human heart at a resolution of 50 ms
Existent-time MRI refers to the continuous imaging of moving objects (such as the heart) in real fourth dimension. 1 of the many different strategies developed since the early on 2000s is based on radial FLASH MRI, and iterative reconstruction. This gives a temporal resolution of 20–30 ms for images with an in-plane resolution of i.five–ii.0 mm.[88] Balanced steady-land gratuitous precession (bSSFP) imaging has a better image dissimilarity betwixt the blood pool and myocardium than the Flash MRI, yet it will produce severe banding antiquity when the B0 inhomogeneity is stiff. Real-fourth dimension MRI is likely to add important information on diseases of the heart and the joints, and in many cases may make MRI examinations easier and more comfy for patients, especially for the patients who cannot concord their breathings or who have arrhythmia.[89]
Interventional MRI [edit]
The lack of harmful effects on the patient and the operator brand MRI well-suited for interventional radiology, where the images produced by an MRI scanner guide minimally invasive procedures. Such procedures utilise no ferromagnetic instruments.[90]
A specialized growing subset of interventional MRI is intraoperative MRI, in which an MRI is used in surgery. Some specialized MRI systems allow imaging concurrent with the surgical procedure. More than typically, the surgical procedure is temporarily interrupted and then that MRI can assess the success of the procedure or guide subsequent surgical work.[91]
Magnetic resonance guided focused ultrasound [edit]
In guided therapy, high-intensity focused ultrasound (HIFU) beams are focused on a tissue, that are controlled using MR thermal imaging. Due to the loftier energy at the focus, the temperature rises to above 65 °C (150 °F) which completely destroys the tissue. This applied science tin can achieve precise ablation of diseased tissue. MR imaging provides a three-dimensional view of the target tissue, allowing for the precise focusing of ultrasound energy. The MR imaging provides quantitative, real-time, thermal images of the treated expanse. This allows the physician to ensure that the temperature generated during each cycle of ultrasound energy is sufficient to cause thermal ablation within the desired tissue and if not, to adapt the parameters to ensure effective handling.[92]
Multinuclear imaging [edit]
Hydrogen has the most frequently imaged nucleus in MRI because information technology is present in biological tissues in great affluence, and because its high gyromagnetic ratio gives a strong betoken. Still, any nucleus with a net nuclear spin could potentially be imaged with MRI. Such nuclei include helium-3, lithium-seven, carbon-13, fluorine-19, oxygen-17, sodium-23, phosphorus-31 and xenon-129. 23Na and 31P are naturally abundant in the body, so they tin be imaged straight. Gaseous isotopes such as 3He or 129Xe must be hyperpolarized and and so inhaled as their nuclear density is too low to yield a useful signal under normal conditions. 17O and 19F can be administered in sufficient quantities in liquid grade (e.g. 17O-water) that hyperpolarization is not a necessity.[93] Using helium or xenon has the reward of reduced groundwork dissonance, and therefore increased contrast for the image itself, because these elements are not usually nowadays in biological tissues.[94]
Moreover, the nucleus of any atom that has a net nuclear spin and that is bonded to a hydrogen atom could potentially be imaged via heteronuclear magnetization transfer MRI that would image the high-gyromagnetic-ratio hydrogen nucleus instead of the low-gyromagnetic-ratio nucleus that is bonded to the hydrogen atom.[95] In principle, heteronuclear magnetization transfer MRI could exist used to discover the presence or absence of specific chemical bonds.[96] [97]
Multinuclear imaging is primarily a research technique at present. All the same, potential applications include functional imaging and imaging of organs poorly seen on aneH MRI (e.grand., lungs and bones) or every bit culling contrast agents. Inhaled hyperpolarized 3He can be used to image the distribution of air spaces within the lungs. Injectable solutions containing 13C or stabilized bubbles of hyperpolarized 129Xe take been studied equally contrast agents for angiography and perfusion imaging. 31P can potentially provide data on bone density and structure, also equally functional imaging of the brain. Multinuclear imaging holds the potential to chart the distribution of lithium in the human encephalon, this element finding utilize as an of import drug for those with conditions such as bipolar disorder.[98]
Molecular imaging by MRI [edit]
MRI has the advantages of having very loftier spatial resolution and is very skillful at morphological imaging and functional imaging. MRI does have several disadvantages though. Outset, MRI has a sensitivity of around ten−3 mol/Fifty to ten−v mol/L, which, compared to other types of imaging, tin be very limiting. This problem stems from the fact that the population difference between the nuclear spin states is very small at room temperature. For instance, at ane.5 teslas, a typical field strength for clinical MRI, the difference between loftier and low energy states is approximately 9 molecules per ii million. Improvements to increment MR sensitivity include increasing magnetic field strength and hyperpolarization via optical pumping or dynamic nuclear polarization. There are too a diversity of signal distension schemes based on chemical commutation that increase sensitivity.[99]
To achieve molecular imaging of disease biomarkers using MRI, targeted MRI dissimilarity agents with high specificity and high relaxivity (sensitivity) are required. To date, many studies take been devoted to developing targeted-MRI contrast agents to achieve molecular imaging by MRI. Normally, peptides, antibodies, or small ligands, and small-scale protein domains, such as HER-2 affibodies, take been applied to accomplish targeting. To enhance the sensitivity of the contrast agents, these targeting moieties are unremarkably linked to high payload MRI dissimilarity agents or MRI dissimilarity agents with high relaxivities.[100] A new class of gene targeting MR contrast agents has been introduced to testify factor action of unique mRNA and gene transcription factor proteins.[101] [102] These new contrast agents can trace cells with unique mRNA, microRNA and virus; tissue response to inflammation in living brains.[103] The MR reports change in gene expression with positive correlation to TaqMan analysis, optical and electron microscopy.[104]
Parallel MRI [edit]
Information technology takes time to assemble MRI data using sequential applications of magnetic field gradients. Fifty-fifty for the nigh streamlined of MRI sequences, in that location are physical and physiologic limits to the charge per unit of gradient switching. Parallel MRI circumvents these limits by gathering some portion of the data simultaneously, rather than in a traditional sequential fashion. This is achieved using arrays of radiofrequency (RF) detector coils, each with a different 'view' of the body. A reduced set of slope steps is applied, and the remaining spatial information is filled in by combining signals from various coils, based on their known spatial sensitivity patterns. The resulting acceleration is limited by the number of coils and by the signal to noise ratio (which decreases with increasing acceleration), but two- to iv-fold accelerations may commonly be achieved with suitable coil array configurations, and substantially higher accelerations have been demonstrated with specialized ringlet arrays. Parallel MRI may be used with about MRI sequences.
After a number of early suggestions for using arrays of detectors to accelerate imaging went largely unremarked in the MRI field, parallel imaging saw widespread development and awarding post-obit the introduction of the SiMultaneous Acquisition of Spatial Harmonics (SMASH) technique in 1996–7.[105] The SENSitivity Encoding (SENSE)[106] and Generalized Autocalibrating Partially Parallel Acquisitions (GRAPPA)[107] techniques are the parallel imaging methods in nearly mutual use today. The advent of parallel MRI resulted in all-encompassing enquiry and development in image reconstruction and RF coil blueprint, also equally in a rapid expansion of the number of receiver channels available on commercial MR systems. Parallel MRI is at present used routinely for MRI examinations in a wide range of body areas and clinical or research applications.
Quantitative MRI [edit]
Most MRI focuses on qualitative interpretation of MR data by acquiring spatial maps of relative variations in signal strength which are "weighted" by certain parameters.[108] Quantitative methods instead attempt to determine spatial maps of accurate tissue relaxometry parameter values or magnetic field, or to measure out the size of certain spatial features.
Examples of quantitative MRI methods are:
- T1-mapping (notably used in cardiac magnetic resonance imaging[109])
- T2-mapping[110]
- Quantitative susceptibility mapping (QSM)
- Quantitative fluid flow MRI (i.e. some cerebrospinal fluid menstruation MRI[111])
- Magnetic resonance elastography (MRE)[112]
Quantitative MRI aims to increment the reproducibility of MR images and interpretations, only has historically suffered from longer required scan times.[108]
Quantitative MRI (or qMRI) sometimes more specifically refers to multi-parametric quantitative MRI, the mapping of multiple tissue relaxometry parameters in a single imaging session.[113] Efforts to make multi-parametric quantitative MRI faster have produced sequences which map multiple parameters simultaneously, either past building separate encoding methods for each parameter into the sequence,[114] or by fitting MR bespeak development to a multi-parameter model.[115] [116]
Safety [edit]
MRI is, in general, a safe technique, although injuries may occur as a upshot of failed safe procedures or human being error.[117] Contraindications to MRI include most cochlear implants and cardiac pacemakers, shrapnel, and metallic foreign bodies in the eyes. Magnetic resonance imaging in pregnancy appears to be safe, at least during the 2nd and 3rd trimesters if done without contrast agents.[118] Since MRI does not use whatever ionizing radiation, its utilize is generally favored in preference to CT when either modality could yield the same information.[119] Some patients experience claustrophobia and may require sedation or shorter MRI protocols.[120] [121] Amplitude and rapid switching of gradient coils during epitome acquisition may cause peripheral nerve stimulation.[122]
MRI uses powerful magnets and can therefore cause magnetic materials to move at bang-up speeds, posing a projectile risk, and may cause fatal accidents.[123] However, as millions of MRIs are performed globally each year,[124] fatalities are extremely rare.[125]
Overuse [edit]
Medical societies issue guidelines for when physicians should use MRI on patients and recommend against overuse. MRI can find health problems or ostend a diagnosis, but medical societies ofttimes recommend that MRI not be the first procedure for creating a programme to diagnose or manage a patient's complaint. A common instance is to utilize MRI to seek a cause of low back pain; the American College of Physicians, for example, recommends against this procedure equally unlikely to result in a positive consequence for the patient.[xv] [sixteen]
Artifacts [edit]

Motion artifact (T1 coronal study of cervical vertebrae)[126]
An MRI artifact is a visual artifact, that is, an bibelot during visual representation. Many different artifacts can occur during magnetic resonance imaging (MRI), some affecting the diagnostic quality, while others may be dislocated with pathology. Artifacts tin be classified equally patient-related, betoken processing-dependent and hardware (machine)-related.[126]
Non-medical use [edit]
MRI is used industrially mainly for routine analysis of chemicals. The nuclear magnetic resonance technique is as well used, for instance, to measure the ratio between water and fat in foods, monitoring of catamenia of corrosive fluids in pipes, or to report molecular structures such as catalysts.[127]
Being non-invasive and non-dissentious, MRI tin exist used to study the beefcake of plants, their water transportation processes and h2o balance.[128] It is besides applied to veterinary radiology for diagnostic purposes. Outside this, its use in zoology is limited due to the loftier cost; only it tin be used on many species.[129]
In palaeontology it is used to examine the construction of fossils.[130]
Forensic imaging provides graphic documentation of an autopsy, which manual autopsy does not. CT scanning provides quick whole-trunk imaging of skeletal and parenchymal alterations, whereas MRI imaging gives better representation of soft tissue pathology.[131] But MRI is more than expensive, and more than fourth dimension-consuming to utilise.[131] Moreover, the quality of MR imaging deteriorates beneath 10 °C.[132]
History [edit]
In 1971 at Stony Brook Academy, Paul Lauterbur applied magnetic field gradients in all three dimensions and a back-project technique to create NMR images. He published the first images of 2 tubes of h2o in 1973 in the journal Nature,[133] followed by the picture of a living beast, a clam, and in 1974 by the paradigm of the thoracic cavity of a mouse. Lauterbur called his imaging method zeugmatography, a term which was replaced by (N)MR imaging.[134] In the late 1970s, physicists Peter Mansfield and Paul Lauterbur developed MRI-related techniques, like the repeat-planar imaging (EPI) technique.[135]
Advances in semiconductor technology were crucial to the evolution of practical MRI, which requires a large amount of computational power. This was made possible by the quickly increasing number of transistors on a single integrated circuit chip.[136] Mansfield and Lauterbur were awarded the 2003 Nobel Prize in Physiology or Medicine for their "discoveries concerning magnetic resonance imaging".[137]
Come across also [edit]
- Physics of magnetic resonance imaging
- Amplified magnetic resonance imaging
- Electron paramagnetic resonance
- High-definition fiber tracking
- High-resolution computed tomography
- History of neuroimaging
- International Society for Magnetic Resonance in Medicine
- Jemris
- List of neuroimaging software
- Magnetic immunoassay
- Magnetic particle imaging
- Magnetic resonance elastography
- Magnetic Resonance Imaging (journal)
- Magnetic resonance microscopy
- Nobel Prize controversies – Physiology or medicine
- Rabi bike
- Robinson oscillator
- Sodium MRI
- Virtopsy
References [edit]
- ^ McRobbie DW, Moore EA, Graves MJ, Prince MR (2007). MRI from Picture to Proton. Cambridge Academy Press. p. i. ISBN978-i-139-45719-iv.
- ^ a b Hoult DI, Bahkar B (1998). "NMR Signal Reception: Virtual Photons and Coherent Spontaneous Emission". Concepts in Magnetic Resonance. 9 (5): 277–297. doi:x.1002/(SICI)1099-0534(1997)9:five<277::Help-CMR1>3.0.CO;ii-W.
- ^ [ irrelevant citation ] Smith-Bindman R, Miglioretti DL, Johnson Due east, Lee C, Feigelson HS, Flynn K, et al. (June 2012). "Apply of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010". JAMA. 307 (22): 2400–ix. doi:10.1001/jama.2012.5960. PMC3859870. PMID 22692172.
- ^ Health at a glance 2009 OECD indicators. Health at a Glance. 2009. doi:10.1787/health_glance-2009-en. ISBN978-92-64-07555-9.
- ^ a b McRobbie DW (2007). MRI from picture to proton. Cambridge, UK; New York: Cambridge University Press. ISBN978-0-521-68384-5.
- ^ Sasaki M, Ehara S, Nakasato T, Tamakawa Y, Kuboya Y, Sugisawa M, Sato T (April 1990). "MR of the shoulder with a 0.2-T permanent-magnet unit of measurement". AJR. American Periodical of Roentgenology. 154 (4): 777–8. doi:10.2214/ajr.154.4.2107675. PMID 2107675.
- ^ "Guildford company gets FDA approval for bedside MRI". New Haven Annals. 12 Feb 2020. Retrieved 15 April 2020.
- ^ McDermott R, Lee S, 10 Haken B, Trabesinger AH, Pines A, Clarke J (May 2004). "Microtesla MRI with a superconducting quantum interference device". Proceedings of the National Academy of Sciences of the U.s.a.. 101 (21): 7857–61. Bibcode:2004PNAS..101.7857M. doi:10.1073/pnas.0402382101. PMC419521. PMID 15141077.
- ^ Zotev VS, Matlashov AN, Volegov PL, Urbaitis AV, Espy MA, Kraus RH (2007). "SQUID-based instrumentation for ultralow-field MRI". Superconductor Science and Engineering. twenty (11): S367–73. arXiv:0705.0661. Bibcode:2007SuScT..20S.367Z. doi:10.1088/0953-2048/xx/11/S13. S2CID 119160258.
- ^ Vesanen PT, Nieminen JO, Zevenhoven KC, Dabek J, Parkkonen LT, Zhdanov AV, et al. (June 2013). "Hybrid ultra-depression-field MRI and magnetoencephalography arrangement based on a commercial whole-head neuromagnetometer". Magnetic Resonance in Medicine. 69 (6): 1795–804. doi:ten.1002/mrm.24413. PMID 22807201. S2CID 40026232.
- ^ a b c d e f g "Magnetic Resonance Imaging". University of Wisconsin. Archived from the original on 2017-05-10. Retrieved 2016-03-14 .
- ^ a b c d e f g h i j k fifty m north Johnson KA. "Basic proton MR imaging. Tissue Point Characteristics". [ unreliable medical source? ]
- ^ a b Patil T (2013-01-18). "MRI sequences". Retrieved 2016-03-14 .
- ^ "Magnetic Resonance, a critical peer-reviewed introduction". European Magnetic Resonance Forum. Retrieved 17 November 2014.
- ^ a b Consumer Reports; American College of Physicians. presented by ABIM Foundation. "5 Things Physicians and Patients Should Question" (PDF). Choosing Wisely. Archived from the original (PDF) on June 24, 2012. Retrieved Baronial 14, 2012.
- ^ a b Consumer Reports; American Higher of Physicians (April 2012). "Imaging tests for lower-dorsum hurting: Why you probably don't demand them" (PDF). High Value Care. Archived from the original (PDF) on 15 January 2013. Retrieved August 14, 2012.
- ^ Husband J (2008). Recommendations for Cross-Exclusive Imaging in Cancer Management: Computed Tomography – CT Magnetic Resonance Imaging – MRI Positron Emission Tomography – PET-CT (PDF). Regal College of Radiologists. ISBN978-1-905034-13-0.
- ^ Heavey Due south, Costa H, Pye H, Burt EC, Jenkinson S, Lewis GR, et al. (May 2019). "PEOPLE: PatiEnt prOstate samPLes for rEsearch, a tissue collection pathway utilizing magnetic resonance imaging data to target tumor and benign tissue in fresh radical prostatectomy specimens". The Prostate. 79 (7): 768–777. doi:10.1002/pros.23782. PMC6618051. PMID 30807665.
- ^ Heavey S, Haider A, Sridhar A, Pye H, Shaw M, Freeman A, Whitaker H (October 2019). "Utilize of Magnetic Resonance Imaging and Biopsy Data to Guide Sampling Procedures for Prostate Cancer Biobanking". Journal of Visualized Experiments (152). doi:x.3791/60216. PMID 31657791.
- ^ American Social club of Neuroradiology (2013). "ACR-ASNR Practice Guideline for the Operation and Interpretation of Magnetic Resonance Imaging (MRI) of the Encephalon" (PDF). Archived from the original (PDF) on 2017-07-12. Retrieved 2013-11-10 .
- ^ Rowayda As (May 2012). "An improved MRI segmentation for atrophy assessment". International Journal of Information science Issues (IJCSI). nine (3).
- ^ Rowayda AS (Feb 2013). "Regional atrophy analysis of MRI for early detection of alzheimer'southward disease". International Journal of Signal Processing, Prototype Processing and Pattern Recognition. vi (1): 49–53.
- ^ Nolen-Hoeksema Southward (2014). Aberrant Psychology (Sixth ed.). New York: McGraw-Hill Educational activity. p. 67.
- ^ Brown RA, Nelson JA (June 2016). "The Invention and Early History of the North-Localizer for Stereotactic Neurosurgery". Cureus. viii (six): e642. doi:10.7759/cureus.642. PMC4959822. PMID 27462476.
- ^ Leksell Fifty, Leksell D, Schwebel J (January 1985). "Stereotaxis and nuclear magnetic resonance". Journal of Neurology, Neurosurgery, and Psychiatry. 48 (i): fourteen–eight. doi:ten.1136/jnnp.48.i.14. PMC1028176. PMID 3882889.
- ^ Heilbrun MP, Sunderland PM, McDonald PR, Wells TH, Cosman E, Ganz E (1987). "Brown-Roberts-Wells stereotactic frame modifications to accomplish magnetic resonance imaging guidance in three planes". Applied Neurophysiology. 50 (one–6): 143–52. doi:ten.1159/000100700. PMID 3329837.
- ^ Kanemaru, Noriko; Takao, Hidemasa; Amemiya, Shiori; Abe, Osamu (2 December 2021). "The effect of a mail-scan processing denoising system on image quality and morphometric analysis". Periodical of Neuroradiology. doi:ten.1016/j.neurad.2021.11.007. PMID 34863809. S2CID 244907903. Retrieved 26 December 2021.
- ^ Petersen SE, Aung N, Sanghvi MM, Zemrak F, Fung K, Paiva JM, et al. (February 2017). "Reference ranges for cardiac construction and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population accomplice". Journal of Cardiovascular Magnetic Resonance. Springer Science and Business Media LLC. 19 (1): eighteen. doi:10.1186/s12968-017-0327-nine. PMC5304550. PMID 28178995.
- ^ American College of Radiology; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; American Society of Nuclear Cardiology; North American Society for Cardiac Imaging; Gild for Cardiovascular Angiography Interventions; Society of Interventional Radiology (October 2006). "ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging. A report of the American College of Cardiology Foundation Quality Strategic Directions Commission Appropriateness Criteria Working Grouping". Journal of the American College of Radiology. iii (10): 751–71. doi:ten.1016/j.jacr.2006.08.008. PMID 17412166.
- ^ Helms C (2008). Musculoskeletal MRI. Saunders. ISBN978-one-4160-5534-ane.
- ^ Aivazoglou, LU; Guimarães, JB; Link, TM; Costa, MAF; Cardoso, FN; de Mattos Lombardi Badia, B; Farias, IB; de Rezende Pinto, WBV; de Souza, PVS; Oliveira, ASB; de Siqueira Carvalho, AA; Aihara, AY; da Rocha Corrêa Fernandes, A (21 April 2021). "MR imaging of inherited myopathies: a review and proposal of imaging algorithms". European Radiology. 31 (11): 8498–8512. doi:x.1007/s00330-021-07931-nine. PMID 33881569. S2CID 233314102.
- ^ Schmidt GP, Reiser MF, Baur-Melnyk A (December 2007). "Whole-body imaging of the musculoskeletal organisation: the value of MR imaging". Skeletal Radiology. Springer Nature. 36 (12): 1109–nineteen. doi:10.1007/s00256-007-0323-5. PMC2042033. PMID 17554538.
- ^ Havsteen I, Ohlhues A, Madsen KH, Nybing JD, Christensen H, Christensen A (2017). "Are Movement Artifacts in Magnetic Resonance Imaging a Real Problem?-A Narrative Review". Frontiers in Neurology. 8: 232. doi:10.3389/fneur.2017.00232. PMC5447676. PMID 28611728.
- ^ Taber, K H; Herrick, R C; Weathers, S W; Kumar, A J; Schomer, D F; Hayman, L A (November 1998). "Pitfalls and artifacts encountered in clinical MR imaging of the spine". RadioGraphics. xviii (6): 1499–1521. doi:10.1148/radiographics.18.half dozen.9821197. ISSN 0271-5333.
- ^ Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, Reeder SB (March 2012). "Hepatobiliary MR imaging with gadolinium-based contrast agents". Journal of Magnetic Resonance Imaging. 35 (3): 492–511. doi:x.1002/jmri.22833. PMC3281562. PMID 22334493.
- ^ Sandrasegaran G, Lin C, Akisik FM, Tann G (July 2010). "State-of-the-fine art pancreatic MRI". AJR. American Journal of Roentgenology. 195 (1): 42–53. doi:x.2214/ajr.195.3_supplement.0s42. PMID 20566796.
- ^ Masselli Chiliad, Gualdi Thou (August 2012). "MR imaging of the small bowel". Radiology. 264 (2): 333–48. doi:ten.1148/radiol.12111658. PMID 22821694.
- ^ Zijta FM, Bipat S, Stoker J (May 2010). "Magnetic resonance (MR) colonography in the detection of colorectal lesions: a systematic review of prospective studies". European Radiology. 20 (5): 1031–46. doi:10.1007/s00330-009-1663-4. PMC2850516. PMID 19936754.
- ^ Wheaton AJ, Miyazaki Thousand (Baronial 2012). "Non-dissimilarity enhanced MR angiography: physical principles". Journal of Magnetic Resonance Imaging. Wiley. 36 (ii): 286–304. doi:10.1002/jmri.23641. PMID 22807222. S2CID 24048799.
- ^ Haacke EM, Brown RF, Thompson M, Venkatesan R (1999). Magnetic resonance imaging: Concrete principles and sequence design. New York: J. Wiley & Sons. ISBN978-0-471-35128-iii. [ folio needed ]
- ^ Rinck PA (2014). "Chapter 13: Contrast Agents". Magnetic Resonance in Medicine.
- ^ Irish potato KJ, Brunberg JA, Cohan RH (Oct 1996). "Adverse reactions to gadolinium contrast media: a review of 36 cases". AJR. American Journal of Roentgenology. 167 (4): 847–ix. doi:10.2214/ajr.167.4.8819369. PMID 8819369.
- ^ "ACR guideline". guideline.gov. 2005. Archived from the original on 2006-09-29. Retrieved 2006-11-22 .
- ^ Sergey Shugaev and Peter Caravan, Affiliate 1: "Metal Ions in Bio-imaging Techniques: A Short Overview", pp ane-37 in "Metal Ions in Bio-Imaging Techniques" (2021). Editors: Astrid Sigel, Eva Freisinger and Roland 1000.O. Sigel. Publisher: Walter de Gruyter, Berlin.
de Gruyter.com/certificate/doi/10.1515/9783110685701-007 DOI 10.1515/9783110685701-007 - ^ "FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new form warnings". United states of america FDA. 2018-05-16.
- ^ Thomsen HS, Morcos SK, Dawson P (November 2006). "Is there a causal relation between the administration of gadolinium based dissimilarity media and the development of nephrogenic systemic fibrosis (NSF)?". Clinical Radiology. 61 (11): 905–6. doi:ten.1016/j.crad.2006.09.003. PMID 17018301.
- ^ "FDA Drug Safe Communication: New warnings for using gadolinium-based dissimilarity agents in patients with kidney dysfunction". Data on Gadolinium-Based Dissimilarity Agents. U.S. Food and Drug Administration. 23 December 2010. Retrieved 12 March 2011.
- ^ "FDA Public Health Advisory: Gadolinium-containing Contrast Agents for Magnetic Resonance Imaging". fda.gov. Archived from the original on 2006-09-28.
- ^ "Gadolinium-containing contrast agents: new advice to minimise the risk of nephrogenic systemic fibrosis". Drug Rubber Update. 3 (half-dozen): 3. Jan 2010.
- ^ "MRI Questions and Answers" (PDF). Hold, CA: International Society for Magnetic Resonance in Medicine. Retrieved 2010-08-02 .
- ^ "Response to the FDA's May 23, 2007, Nephrogenic Systemic Fibrosis Update1 — Radiology". Radiological Society of North America. 2007-09-12. Archived from the original on 2012-07-xix. Retrieved 2010-08-02 .
- ^ Jones J, Gaillard F. "MRI sequences (overview)". Radiopaedia . Retrieved 2017-10-15 .
- ^ a b c d "Magnetic Resonance Imaging". Academy of Wisconsin. Archived from the original on 2017-05-10. Retrieved 2016-03-14 .
- ^ a b c d Johnson KA. "Basic proton MR imaging. Tissue Signal Characteristics". Harvard Medical Schoolhouse. Archived from the original on 2016-03-05. Retrieved 2016-03-14 .
- ^ "MRI Questions, Fast Spin Echo". MRIQuestions.com. Retrieved 2021-05-xviii .
- ^ Graham D, Cloke P, Vosper M (2011-05-31). Principles and Applications of Radiological Physics Due east-Book (half-dozen ed.). Elsevier Health Sciences. p. 292. ISBN978-0-7020-4614-eight. }
- ^ du Plessis V, Jones J. "MRI sequences (overview)". Radiopaedia . Retrieved 2017-01-13 .
- ^ Lefevre N, Naouri JF, Herman S, Gerometta A, Klouche S, Bohu Y (2016). "A Current Review of the Meniscus Imaging: Proposition of a Useful Tool for Its Radiologic Analysis". Radiology Inquiry and Practice. 2016: 8329296. doi:10.1155/2016/8329296. PMC4766355. PMID 27057352.
- ^ a b Luijkx T, Weerakkody Y. "Steady-state free precession MRI". Radiopaedia . Retrieved 2017-10-thirteen .
- ^ a b Chavhan GB, Babyn PS, Thomas B, Shroff MM, Haacke EM (2009). "Principles, techniques, and applications of T2*-based MR imaging and its special applications". Radiographics. 29 (5): 1433–49. doi:10.1148/rg.295095034. PMC2799958. PMID 19755604.
- ^ a b Di Muzio B, Gaillard F. "Susceptibility weighted imaging". Retrieved 2017-10-15 .
- ^ Sharma R, Taghi Niknejad M. "Short tau inversion recovery". Radiopaedia . Retrieved 2017-10-13 .
- ^ Berger F, de Jonge M, Smithuis R, Maas M. "Stress fractures". Radiology Assistant. Radiology Society of the Netherlands. Retrieved 2017-10-xiii .
- ^ Hacking C, Taghi Niknejad M, et al. "Fluid attenuation inversion recoveryg". radiopaedia.org . Retrieved 2015-12-03 .
- ^ a b Di Muzio B, Abd Rabou A. "Double inversion recovery sequence". Radiopaedia . Retrieved 2017-10-13 .
- ^ Lee M, Bashir U. "Diffusion weighted imaging". Radiopaedia . Retrieved 2017-10-thirteen .
- ^ Weerakkody Y, Gaillard F. "Ischaemic stroke". Radiopaedia . Retrieved 2017-10-15 .
- ^ Hammer Chiliad. "MRI Physics: Diffusion-Weighted Imaging". XRayPhysics . Retrieved 2017-10-15 .
- ^ An H, Ford AL, Vo One thousand, Powers WJ, Lee JM, Lin W (May 2011). "Signal development and infarction risk for credible improvidence coefficient lesions in astute ischemic stroke are both time- and perfusion-dependent". Stroke. 42 (5): 1276–81. doi:10.1161/STROKEAHA.110.610501. PMC3384724. PMID 21454821.
- ^ a b Smith D, Bashir U. "Improvidence tensor imaging". Radiopaedia . Retrieved 2017-x-13 .
- ^ Chua TC, Wen Westward, Slavin MJ, Sachdev PS (February 2008). "Diffusion tensor imaging in mild cognitive impairment and Alzheimer'due south affliction: a review". Current Opinion in Neurology. 21 (1): 83–92. doi:10.1097/WCO.0b013e3282f4594b. PMID 18180656.
- ^ Gaillard F. "Dynamic susceptibility contrast (DSC) MR perfusion". Radiopaedia . Retrieved 2017-10-14 .
- ^ Chen F, Ni YC (March 2012). "Magnetic resonance diffusion-perfusion mismatch in astute ischemic stroke: An update". Earth Journal of Radiology. 4 (3): 63–74. doi:10.4329/wjr.v4.i3.63. PMC3314930. PMID 22468186.
- ^ "Arterial spin labeling". University of Michigan . Retrieved 2017-10-27 .
- ^ Gaillard F. "Arterial spin labelling (ASL) MR perfusion". Radiopaedia . Retrieved 2017-10-15 .
- ^ Gaillard F. "Dynamic contrast enhanced (DCE) MR perfusion". Radiopaedia . Retrieved 2017-x-15 .
- ^ Turnbull LW (January 2009). "Dynamic contrast-enhanced MRI in the diagnosis and management of chest cancer". NMR in Biomedicine. 22 (1): 28–39. doi:10.1002/nbm.1273. PMID 18654999.
- ^ Chou I. "Milestone nineteen: (1990) Functional MRI". Nature. Retrieved 9 Baronial 2013.
- ^ Luijkx T, Gaillard F. "Functional MRI". Radiopaedia . Retrieved 2017-ten-sixteen .
- ^ a b "Magnetic Resonance Angiography (MRA)". Johns Hopkins Hospital . Retrieved 2017-ten-15 .
- ^ Keshavamurthy J, Ballinger R et al. "Phase contrast imaging". Radiopaedia . Retrieved 2017-x-15 .
- ^ Landheer Yard, Schulte RF, Treacy MS, Swanberg KM, Juchem C (Apr 2020). "Theoretical description of modernistic 1 H in Vivo magnetic resonance spectroscopic pulse sequences". Journal of Magnetic Resonance Imaging. 51 (4): 1008–1029. doi:x.1002/jmri.26846. PMID 31273880. S2CID 195806833.
- ^ Rosen Y, Lenkinski RE (July 2007). "Contempo advances in magnetic resonance neurospectroscopy". Neurotherapeutics. 4 (3): 330–45. doi:10.1016/j.nurt.2007.04.009. PMC7479727. PMID 17599700.
- ^ Golder W (June 2004). "Magnetic resonance spectroscopy in clinical oncology". Onkologie. 27 (three): 304–9. doi:ten.1159/000077983. PMID 15249722. S2CID 20644834.
- ^ Chakeres DW, Abduljalil AM, Novak P, Novak V (2002). "Comparison of one.5 and viii tesla loftier-resolution magnetic resonance imaging of lacunar infarcts". Journal of Computer Assisted Tomography. 26 (four): 628–32. doi:10.1097/00004728-200207000-00027. PMID 12218832. S2CID 32536398.
- ^ "MRI-scanner van vii miljoen in gebruik" [MRI scanner of €7 million in employ] (in Dutch). Medisch Contact. December 5, 2007.
- ^ Abeida H, Zhang Q, Li J, Merabtine North (2013). "Iterative Sparse Asymptotic Minimum Variance Based Approaches for Array Processing". IEEE Transactions on Point Processing. 61 (4): 933–44. arXiv:1802.03070. Bibcode:2013ITSP...61..933A. doi:10.1109/tsp.2012.2231676. S2CID 16276001.
- ^ Uecker Yard, Zhang S, Voit D, Karaus A, Merboldt KD, Frahm J (October 2010). "Real-fourth dimension MRI at a resolution of 20 ms". NMR in Biomedicine. 23 (viii): 986–94. doi:10.1002/nbm.1585. hdl:11858/00-001M-0000-0012-D4F9-7. PMID 20799371. S2CID 8268489.
- ^ Uyanik I, Lindner P, Tsiamyrtzis P, Shah D, Tsekos NV, Pavlidis Information technology (2013). Functional Imaging and Modeling of the Middle. Lecture Notes in Computer Science. Vol. 7945. pp. 466–473. doi:10.1007/978-3-642-38899-6_55. ISBN978-3-642-38898-9. ISSN 0302-9743. S2CID 16840737.
- ^ Lewin JS (May 1999). "Interventional MR imaging: concepts, systems, and applications in neuroradiology". AJNR. American Journal of Neuroradiology. xx (5): 735–48. PMC7056143. PMID 10369339.
- ^ Sisk JE (2013). The Gale Encyclopedia of Nursing and Allied Health (3rd ed.). Farmington, MI: Gale. ISBN9781414498881 – via Credo Reference.
- ^ Cline HE, Schenck JF, Hynynen K, Watkins RD, Souza SP, Jolesz FA (1992). "MR-guided focused ultrasound surgery". Periodical of Figurer Assisted Tomography. 16 (6): 956–65. doi:10.1097/00004728-199211000-00024. PMID 1430448.
- ^ Gore JC, Yankeelov TE, Peterson TE, Avison MJ (June 2009). "Molecular imaging without radiopharmaceuticals?". Journal of Nuclear Medicine. Society of Nuclear Medicine. fifty (half-dozen): 999–1007. doi:10.2967/jnumed.108.059576. PMC2719757. PMID 19443583.
- ^ "Hyperpolarized Element of group 0 MRI Laboratory: Hyperpolarized Xenon MR Imaging of the Brain". Harvard Medical School. Archived from the original on 2018-09-20. Retrieved 2017-07-26 .
- ^ Hurd RE, John BK (1991). "Gradient-enhanced proton-detected heteronuclear multiple-breakthrough coherence spectroscopy". Journal of Magnetic Resonance. 91 (3): 648–53. Bibcode:1991JMagR..91..648H. doi:ten.1016/0022-2364(91)90395-a.
- ^ Brownish RA, Venters RA, Tang PP, Spicer LD (1995). "A Test for Scaler Coupling between Heteronuclei Using Slope-Enhanced Proton-Detected HMQC Spectroscopy". Periodical of Magnetic Resonance, Series A. 113 (1): 117–19. Bibcode:1995JMagR.113..117B. doi:10.1006/jmra.1995.1064.
- ^ Miller AF, Egan LA, Townsend CA (March 1997). "Measurement of the degree of coupled isotopic enrichment of different positions in an antibiotic peptide by NMR". Periodical of Magnetic Resonance. 125 (1): 120–31. Bibcode:1997JMagR.125..120M. doi:x.1006/jmre.1997.1107. PMID 9245367. S2CID 14022996.
- ^ Necus J, Sinha N, Smith Atomic number 26, Thelwall PE, Flowers CJ, Taylor PN, et al. (June 2019). "White matter microstructural properties in bipolar disorder in relationship to the spatial distribution of lithium in the brain". Periodical of Melancholia Disorders. 253: 224–231. doi:10.1016/j.jad.2019.04.075. PMC6609924. PMID 31054448.
- ^ Gallagher FA (July 2010). "An introduction to functional and molecular imaging with MRI". Clinical Radiology. 65 (7): 557–66. doi:x.1016/j.crad.2010.04.006. PMID 20541655.
- ^ Xue Due south, Qiao J, Pu F, Cameron M, Yang JJ (2013). "Blueprint of a novel course of poly peptide-based magnetic resonance imaging dissimilarity agents for the molecular imaging of cancer biomarkers". Wiley Interdisciplinary Reviews. Nanomedicine and Nanobiotechnology. 5 (2): 163–79. doi:10.1002/wnan.1205. PMC4011496. PMID 23335551.
- ^ Liu CH, Kim Year, Ren JQ, Eichler F, Rosen BR, Liu PK (January 2007). "Imaging cerebral gene transcripts in alive animals". The Journal of Neuroscience. 27 (three): 713–22. doi:10.1523/JNEUROSCI.4660-06.2007. PMC2647966. PMID 17234603.
- ^ Liu CH, Ren J, Liu CM, Liu PK (Jan 2014). "Intracellular gene transcription factor protein-guided MRI past Deoxyribonucleic acid aptamers in vivo". FASEB Journal. 28 (ane): 464–73. doi:10.1096/fj.13-234229. PMC3868842. PMID 24115049.
- ^ Liu CH, You Z, Liu CM, Kim YR, Whalen MJ, Rosen BR, Liu PK (March 2009). "Diffusion-weighted magnetic resonance imaging reversal by gene knockdown of matrix metalloproteinase-9 activities in alive beast brains". The Journal of Neuroscience. 29 (11): 3508–17. doi:10.1523/JNEUROSCI.5332-08.2009. PMC2726707. PMID 19295156.
- ^ Liu CH, Yang J, Ren JQ, Liu CM, You Z, Liu PK (February 2013). "MRI reveals differential effects of amphetamine exposure on neuroglia in vivo". FASEB Periodical. 27 (2): 712–24. doi:10.1096/fj.12-220061. PMC3545538. PMID 23150521.
- ^ Sodickson DK, Manning WJ (October 1997). "Simultaneous acquisition of spatial harmonics (SMASH): fast imaging with radiofrequency scroll arrays". Magnetic Resonance in Medicine. 38 (iv): 591–603. doi:10.1002/mrm.1910380414. PMID 9324327. S2CID 17505246.
- ^ Pruessmann KP, Weiger Thousand, Scheidegger MB, Boesiger P (Nov 1999). "SENSE: sensitivity encoding for fast MRI". Magnetic Resonance in Medicine. 42 (5): 952–62. doi:10.1002/(SICI)1522-2594(199911)42:5<952::AID-MRM16>3.0.CO;2-S. PMID 10542355.
- ^ Griswold MA, Jakob PM, Heidemann RM, Nittka G, Jellus V, Wang J, Kiefer B, Haase A (June 2002). "Generalized autocalibrating partially parallel acquisitions (GRAPPA)". Magnetic Resonance in Medicine. 47 (vi): 1202–10. doi:ten.1002/mrm.10171. PMID 12111967. S2CID 14724155.
- ^ a b Gulani, Vikas & Nicole, Sieberlich (2020). "Quantitative MRI: Rationale and Challenges". Quantitative Magnetic Resonance Imaging. Academic Press. p. xxxvii-li. doi:10.1016/B978-0-12-817057-1.00001-9. ISBN9780128170571. S2CID 234995365.
- ^ Captur Thou, Manisty C, Moon JC (2016). "Cardiac MRI evaluation of myocardial disease". Middle. 102 (eighteen): 1429–35. doi:10.1136/heartjnl-2015-309077. PMID 27354273. S2CID 23647168.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cobianchi Bellisari F, De Marino 50, Arrigoni F, Mariani S, Bruno F, Palumbo P; et al. (2021). "T2-mapping MRI evaluation of patellofemoral cartilage in patients submitted to intra-articular platelet-rich plasma (PRP) injections". Radiol Med. 126 (viii): 1085–1094. doi:ten.1007/s11547-021-01372-6. PMC8292236. PMID 34008045.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gaillard, Frank. "CSF flow studies | Radiology Reference Article | Radiopaedia.org". Radiopaedia . Retrieved 2021-xi-24 .
- ^ Hirsch, Sebastian; Braun, Jürgen; Sack, Ingolf (2016). Magnetic Resonance Elastography | Wiley Online Books. doi:10.1002/9783527696017. ISBN9783527696017.
- ^ Seiler A, Nöth U, Hok P, Reiländer A, Maiworm M, Baudrexel South; et al. (2021). "Multiparametric Quantitative MRI in Neurological Diseases". Front Neurol. 12: 640239. doi:10.3389/fneur.2021.640239. PMC7982527. PMID 33763021.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Warntjes JB, Leinhard OD, West J, Lundberg P (2008). "Rapid magnetic resonance quantification on the brain: Optimization for clinical usage". Magn Reson Med. threescore (2): 320–9. doi:x.1002/mrm.21635. PMID 18666127. S2CID 11617224.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ehses P, Seiberlich Northward, Ma D, Breuer FA, Jakob PM, Griswold MA; et al. (2013). "IR TrueFISP with a gilt-ratio-based radial readout: fast quantification of T1, T2, and proton density". Magn Reson Med. 69 (one): 71–81. doi:x.1002/mrm.24225. PMID 22378141. S2CID 24244167.
{{cite periodical}}: CS1 maint: multiple names: authors list (link) - ^ Ma D, Gulani Five, Seiberlich N, Liu One thousand, Sunshine JL, Duerk JL; et al. (2013). "Magnetic resonance fingerprinting". Nature. 495 (7440): 187–92. Bibcode:2013Natur.495..187M. doi:10.1038/nature11971. PMC3602925. PMID 23486058.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Watson RE (2015). "Lessons Learned from MRI Safety Events". Current Radiology Reports. three (10). doi:10.1007/s40134-015-0122-z. S2CID 57880401.
- ^ Mervak BM, Altun Eastward, McGinty KA, Hyslop WB, Semelka RC, Burke LM (March 2019). "MRI in pregnancy: Indications and applied considerations". Periodical of Magnetic Resonance Imaging. 49 (3): 621–631. doi:x.1002/jmri.26317. PMID 30701610. S2CID 73412175.
- ^ "iRefer". Royal College of Radiologists. Retrieved ten November 2013.
- ^ Tater KJ, Brunberg JA (1997). "Adult claustrophobia, anxiety and sedation in MRI". Magnetic Resonance Imaging. Elsevier BV. xv (1): 51–four. doi:ten.1016/s0730-725x(96)00351-7. PMID 9084025.
- ^ Shahrouki, Puja; Nguyen, Kim-Lien; Moriarty, John M.; Plotnik, Adam N.; Yoshida, Takegawa; Finn, J. Paul (2021-09-01). "Minimizing tabular array fourth dimension in patients with claustrophobia using focused ferumoxytol-enhanced MR angiography ( f -FEMRA): a feasibility study". The British Periodical of Radiology. 94 (1125): 20210430. doi:x.1259/bjr.20210430. ISSN 0007-1285. PMID 34415199.
- ^ Klein V, Davids Thousand, Schad LR, Wald LL, Guérin B (February 2021). "Investigating cardiac stimulation limits of MRI slope coils using electromagnetic and electrophysiological simulations in man and canine trunk models". Magnetic Resonance in Medicine. 85 (2): 1047–1061. doi:x.1002/mrm.28472. PMC7722025. PMID 32812280.
- ^ Agence France-Presse (30 Jan 2018). "Man dies after being sucked into MRI scanner at Indian infirmary". The Guardian.
- ^ "Magnetic Resonance Imaging (MRI) Exams per 1,000 Population, 2014". OECD. 2016.
- ^ Mansouri M, Aran S, Harvey HB, Shaqdan KW, Abujudeh HH (April 2016). "Rates of safety incident reporting in MRI in a large bookish medical center". Journal of Magnetic Resonance Imaging. John Wiley and Sons. 43 (four): 998–1007. doi:10.1002/jmri.25055. PMID 26483127. S2CID 25245904.
- ^ a b Erasmus LJ, Hurter D, Naude Thou, Kritzinger HG, Acho S (2004). "A short overview of MRI artefacts". South African Journal of Radiology. 8 (2): 13. doi:10.4102/sajr.v8i2.127.
- ^ Rinck PA (2017). "Chapter Nineteen Non-Medical Applications of NMR and MRI". Magnetic Resonance (11th ed.). Retrieved 2017-12-eighteen .
- ^ Van As H (2006-11-xxx). "Intact plant MRI for the written report of cell h2o relations, membrane permeability, jail cell-to-cell and long altitude water transport". Journal of Experimental Botany. Oxford University Press (OUP). 58 (four): 743–56. doi:10.1093/jxb/erl157. PMID 17175554.
- ^ Ziegler A, Kunth M, Mueller S, Bock C, Pohmann R, Schröder Fifty, Faber C, Giribet G (2011-10-xiii). "Application of magnetic resonance imaging in zoology". Zoomorphology. Springer Science and Business concern Media LLC. 130 (four): 227–254. doi:10.1007/s00435-011-0138-8. hdl:11858/00-001M-0000-0013-B8B0-B. ISSN 0720-213X. S2CID 43555012.
- ^ Giovannetti G, Guerrini A, Salvadori PA (July 2016). "Magnetic resonance spectroscopy and imaging for the study of fossils". Magnetic Resonance Imaging. Elsevier BV. 34 (half dozen): 730–742. doi:10.1016/j.mri.2016.03.010. PMID 26979538.
- ^ a b Filograna 50, Pugliese L, Muto M, Tatulli D, Guglielmi K, Thali MJ, Floris R (February 2019). "A Practical Guide to Virtual Autopsy: Why, When and How". Seminars in Ultrasound, CT, and MR. 40 (ane): 56–66. doi:10.1053/j.sult.2018.10.011. PMID 30686369. S2CID 59304740.
- ^ Ruder TD, Thali MJ, Hatch GM (April 2014). "Essentials of forensic mail-mortem MR imaging in adults". The British Journal of Radiology. 87 (1036): 20130567. doi:x.1259/bjr.20130567. PMC4067017. PMID 24191122.
- ^ LAUTERBUR, P. C. (1973). "Prototype Formation by Induced Local Interactions: Examples Employing Nuclear Magnetic Resonance". Nature. Springer Science and Business organization Media LLC. 242 (5394): 190–191. Bibcode:1973Natur.242..190L. doi:10.1038/242190a0. ISSN 0028-0836. S2CID 4176060.
- ^ Rinck PA (2008). "A short history of magnetic resonance imaging". Spectroscopy Europe. 20 (1): seven.
- ^ Mansfield P, Grannell PK (1975). ""Diffraction" and microscopy in solids and liquids by NMR". Physical Review B. 12 (9): 3618–34. Bibcode:1975PhRvB..12.3618M. doi:ten.1103/physrevb.12.3618.
- ^ Rosenblum B, Kuttner F (2011). Breakthrough Enigma: Physics Encounters Consciousness. Oxford University Press. p. 127. ISBN9780199792955.
- ^ "The Nobel Prize in Physiology or Medicine 2003". Nobel Foundation. Archived from the original on eighteen July 2007. Retrieved 28 July 2007.
Further reading [edit]
- Rinck PA (ed.). "The history of MRI". TRTF/EMRF.
- Eustace SJ, Nelson E (June 2004). "Whole torso magnetic resonance imaging". BMJ. 328 (7453): 1387–eight. doi:ten.1136/bmj.328.7453.1387. PMC421763. PMID 15191954.
- Sakr, HM; Fahmy, Due north; Elsayed, NS; Abdulhady, H; El-Sobky, TA; Saadawy, AM; Beroud, C; Udd, B (1 July 2021). "Whole-body musculus MRI characteristics of LAMA2-related congenital muscular dystrophy children: An emerging design". Neuromuscular Disorders. 31 (9): 814–823. doi:ten.1016/j.nmd.2021.06.012. PMID 34481707. S2CID 235691786.
- Pykett IL (May 1982). "NMR imaging in medicine". Scientific American. 246 (v): 78–88. Bibcode:1982SciAm.246e..78P. doi:ten.1038/scientificamerican0582-78. PMID 7079720.
- Simon K, Mattson JS (1996). The pioneers of NMR and magnetic resonance in medicine: The story of MRI. Ramat Gan, Israel: Bar-Ilan Academy Press. ISBN978-0-9619243-ane-7.
- Haacke EM, Brown RF, Thompson One thousand, Venkatesan R (1999). Magnetic resonance imaging: Physical principles and sequence pattern. New York: J. Wiley & Sons. ISBN978-0-471-35128-3.
- Lee SC, Kim G, Kim J, Lee Southward, Han Yi J, Kim SW, et al. (June 2001). "One micrometer resolution NMR microscopy". Journal of Magnetic Resonance. 150 (2): 207–xiii. Bibcode:2001JMagR.150..207L. doi:10.1006/jmre.2001.2319. PMID 11384182.
- Sprawls P (2000). Magnetic Resonance Imaging Principles, Methods, and Techniques . Medical Physics Publishing. ISBN978-0-944838-97-6.
- Mansfield P (1982). NMR Imaging in Biomedicine: Supplement 2 Advances in Magnetic Resonance. Elsevier. ISBN978-0-323-15406-2.
- Fukushima Eastward (1989). NMR in Biomedicine: The Physical Basis. Springer Science & Business organisation Media. ISBN978-0-88318-609-1.
- Blümich B, Kuhn W (1992). Magnetic Resonance Microscopy: Methods and Applications in Materials Scientific discipline, Agronomics and Biomedicine. Wiley. ISBN978-3-527-28403-0.
- Blümer P (1998). Blümler P, Blümich B, Botto RE, Fukushima Due east (eds.). Spatially Resolved Magnetic Resonance: Methods, Materials, Medicine, Biological science, Rheology, Geology, Ecology, Hardware. Wiley-VCH. ISBN978-iii-527-29637-8.
- Liang Z, Lauterbur PC (1999). Principles of Magnetic Resonance Imaging: A Signal Processing Perspective. Wiley. ISBN978-0-7803-4723-half-dozen.
- Schmitt F, Stehling MK, Turner R (1998). Echo-Planar Imaging: Theory, Technique and Application. Springer Berlin Heidelberg. ISBN978-3-540-63194-1.
- Kuperman V (2000). Magnetic Resonance Imaging: Concrete Principles and Applications. Academic Printing. ISBN978-0-08-053570-8.
- Blümich B (2000). NMR Imaging of Materials. Clarendon Printing. ISBN978-0-19-850683-half dozen.
- Jin J (1998). Electromagnetic Analysis and Blueprint in Magnetic Resonance Imaging. CRC Press. ISBN978-0-8493-9693-nine.
- Farhat IA, Belton P, Webb GA (2007). Magnetic Resonance in Food Scientific discipline: From Molecules to Human. Royal Society of Chemistry. ISBN978-0-85404-340-8.
External links [edit]
- Rinck PA (ed.). "MRI: A Peer-Reviewed, Critical Introduction". European Magnetic Resonance Forum (EMRF)/The Circular Table Foundation (TRTF).
- A Guided Bout of MRI: An introduction for laypeople National High Magnetic Field Laboratory
- The Basics of MRI. Underlying physics and technical aspects.
- Video: What to Expect During Your MRI Test from the Institute for Magnetic Resonance Safety, Teaching, and Research (IMRSER)
- Royal Institution Lecture – MRI: A Window on the Human Body
- A Short History of Magnetic Resonance Imaging from a European Point of View
- How MRI works explained just using diagrams
- Real-time MRI videos: Biomedizinische NMR Forschungs GmbH.
- Paul C. Lauterbur, Genesis of the MRI (Magnetic Resonance Imaging) notebook, September 1971 (all pages freely available for download in variety of formats from Science History Institute Digital Collections at digital.sciencehistory.org)


0 Response to "Mri Scanner Is Controlled by Computer Hardware"
Post a Comment